You're not imagining it.
If you're eating less, moving more, and the scale is still creeping up — especially around your middle — I want you to know: this isn't in your head, and it's definitely not a lack of willpower.
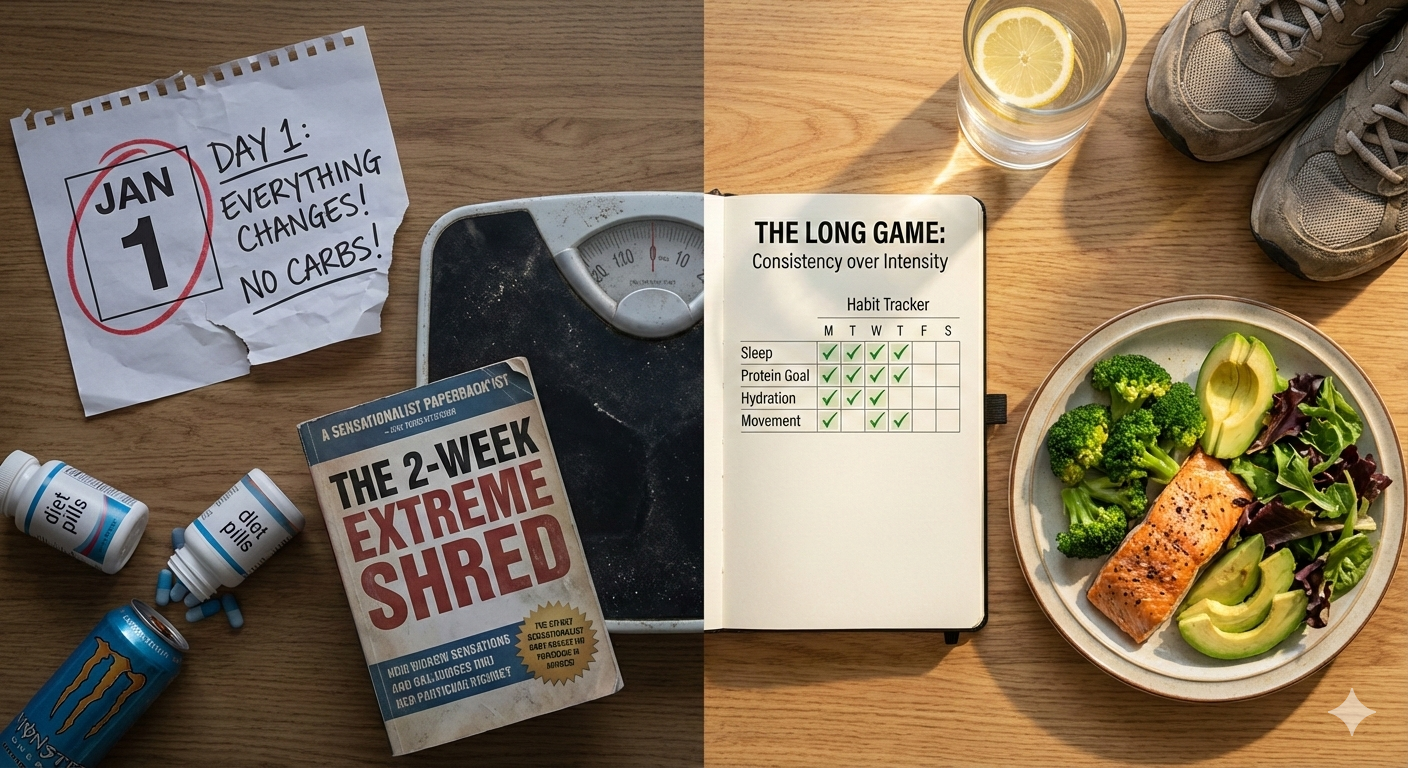
For so many women in their late 30s, 40s, and early 50s, the same strategies that worked for years suddenly stop delivering. You're counting calories, skipping meals, pushing through workouts... and you're exhausted, frustrated, and stuck.
This isn't about what you're doing wrong. It's about your body changing — and needing a different approach now.
Why "Eat Less, Move More" Stops Working
Calories don't tell the whole story. They don't tell us how your hormones are functioning, whether your blood sugar is stable, if your stress response is running on overdrive, or how much muscle you're carrying.
In perimenopause, your hormones, muscle mass, sleep, and stress levels dramatically change how many calories you burn, how hungry you feel, and whether those calories get burned or stored as fat.
The Four Big Shifts Happening in Your Body
1. Estrogen changes fat storage
As estrogen fluctuates and drops, your body becomes more insulin resistant and starts storing fat around your middle — even if you haven't changed how much you're eating. This is especially true when combined with poor sleep, stress, or refined carbs.
2. Eating less can backfire
When you chronically under-eat, your body interprets it as stress. It responds by cranking up hunger, making blood sugar erratic, breaking down muscle, and lowering your metabolic rate.
Sound familiar? Waking at 2am with racing thoughts. Afternoon energy crashes. Intense evening cravings. Stubborn belly fat that won't budge. These aren't signs you're failing — they're signs your body feels under threat.
3. Muscle loss tanks your metabolism
From your mid-30s onward, you naturally lose muscle unless you actively preserve it. In perimenopause, this accelerates. When you cut calories without enough protein and strength training, you lose muscle along with fat — and end up eating less while burning less at the same time.
4. Blood sugar chaos drives cravings and fat storage
Hormonal changes make blood sugar control more fragile. Unstable blood sugar means feeling "hangry," energy crashes, intense carb cravings, and more fat storage around your midsection. Calorie counting doesn't address this — and it's often the missing piece.
What to Focus On Instead
Sustainable weight loss in perimenopause requires a hormone-aware approach, not endless restriction:
Eat enough protein — Aim for protein at each meal (around 1.0-1.2g per kg of body weight daily for most women) to preserve muscle.
Balance your meals — Combine protein, fiber, healthy fats, and lower-glycemic carbs to stabilize blood sugar. Avoid under-eating all day then overeating at night.
Support your stress response — Prioritize sleep and nervous system regulation. Keep training realistic. When your body doesn't feel threatened, it's far more willing to release stored fat.
Get the right tests — If you have extreme fatigue, hair changes, irregular cycles, or significant belly weight gain, check your thyroid and metabolic health.
Create safety for your nervous system — Consistent meals, adequate fuel, and recovery tell your body it's safe to let go of stored energy.
When these systems are supported, a moderate calorie deficit becomes far more effective — and weight loss can happen without extreme restriction.
The Bottom Line
If "eat less and exercise more" has stopped working, you're not failing. Your body has changed, and it needs a different strategy.
Weight loss after 35 isn't about eating less and less. It's about working with your physiology — your hormones, muscle, metabolism, stress, and blood sugar — so a gentle energy deficit actually delivers results.
You deserve an approach that honors what your body is going through, not one that fights against it.
Want to know exactly what's blocking your weight loss? I've created a free Metabolism Detective Quiz to help you uncover what's really happening with your metabolism, hormones, and stress response. Head to the home page of my website and look for the ‘Metabolism Detective” tab to download your free quiz. In just a few minutes, you'll get personalized insights into which metabolic pattern you're stuck in — and the exact steps you need to take to finally start seeing results again.